Contraindications for Manual Lymphatic Drainage: A Comprehensive Guide
Manual Lymphatic Drainage (MLD) presents specific contraindications, including acute infections, severe cardiac issues, and active malignant tumors; careful assessment is crucial․
I․ Absolute Contraindications
Absolute contraindications for Manual Lymphatic Drainage (MLD) signify conditions where the therapy should never be performed due to potential harm․ Acute infections, such as acute cellulitis & erysipelas, and acute lymphangitis, pose significant risks, as MLD could spread the infection․ Similarly, any active localized infection is a firm no․
Severe cardiovascular conditions, including severe cardiac insufficiency and unstable angina, are absolute contraindications because MLD can place undue stress on the heart․ The presence of acute thrombophlebitis – inflammation of a vein with a blood clot – also prohibits MLD, as it could dislodge the clot․ These conditions demand prioritizing conventional medical treatment over lymphatic drainage․
A․ Acute Infections
Acute infections represent a critical contraindication for Manual Lymphatic Drainage (MLD)․ Conditions like acute cellulitis & erysipelas, bacterial skin infections, are strictly prohibited, as MLD could exacerbate the spread of pathogens throughout the lymphatic system․ Acute lymphangitis, inflammation of the lymphatic vessels, also necessitates avoiding MLD․
Furthermore, any active localized infection – regardless of origin – is an absolute reason to postpone or avoid MLD․ The gentle, rhythmic movements of MLD can stimulate circulation, potentially disseminating the infection to previously unaffected areas․ Prioritizing treatment of the infection itself is paramount before considering lymphatic drainage techniques․
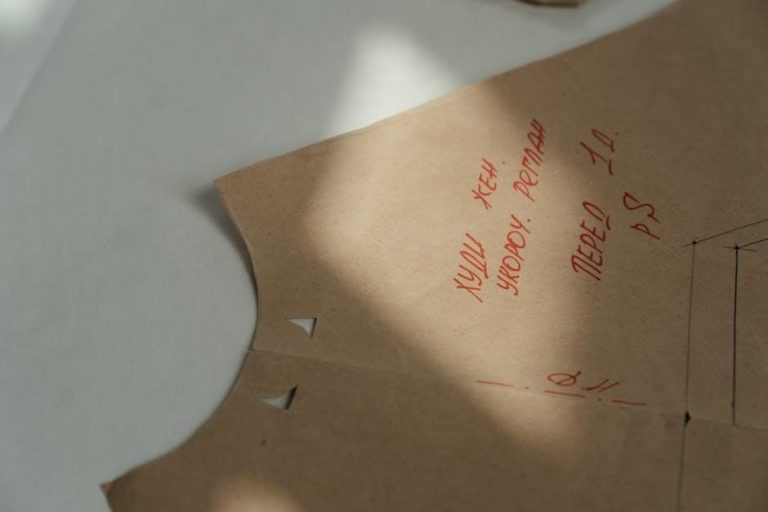
Acute Cellulitis & Erysipelas
Acute cellulitis and erysipelas are bacterial skin infections presenting as significant contraindications to Manual Lymphatic Drainage (MLD)․ These conditions involve inflammation and infection of the deeper skin layers and superficial lymphatics, respectively․ Applying MLD could potentially worsen the infection by mobilizing bacteria through the lymphatic vessels․
The risk lies in spreading the infection beyond the initial site, leading to systemic complications․ MLD’s focus on fluid movement could inadvertently accelerate bacterial dissemination․ Treatment should prioritize antibiotic therapy and addressing the underlying infection before any lymphatic techniques are considered․ MLD is absolutely contraindicated until the infection is fully resolved and cleared by a medical professional․
Acute Lymphangitis

Acute lymphangitis, an inflammation of the lymphatic vessels, represents a firm contraindication for Manual Lymphatic Drainage (MLD)․ Typically caused by bacterial infection, it manifests as red streaks extending from an infected wound, indicating lymphatic involvement․ Applying MLD in this scenario could exacerbate the inflammatory process and propel the infection further into the lymphatic system․
The manipulation inherent in MLD risks dislodging infectious agents and accelerating their spread, potentially leading to lymphadenitis or even sepsis․ Prioritizing antibiotic treatment to resolve the underlying infection is paramount․ MLD should only be considered after complete resolution of the acute inflammation and confirmation by a healthcare provider that the infection is eradicated, ensuring patient safety․
Active Localized Infection
Active localized infections, such as abscesses, boils, or infected wounds, are absolute contraindications for Manual Lymphatic Drainage (MLD)․ Introducing lymphatic drainage techniques to an area harboring an active infection poses a significant risk of disseminating the pathogens throughout the lymphatic network․ This can lead to a widespread infection, potentially causing systemic complications․
MLD’s gentle, rhythmic movements can inadvertently mobilize bacteria or viruses, accelerating their spread to previously unaffected areas․ Treatment should focus on resolving the infection through appropriate medical intervention – typically antibiotics or drainage of the abscess․ MLD can only be contemplated once the infection is fully resolved and the area is demonstrably free from active inflammation, as confirmed by a healthcare professional․
B․ Severe Cardiovascular Conditions
Severe cardiovascular conditions represent a critical set of contraindications for Manual Lymphatic Drainage (MLD)․ Conditions like severe cardiac insufficiency and unstable angina place undue stress on an already compromised circulatory system․ MLD, while gentle, still involves fluid shifts that the heart may be unable to effectively manage․
Furthermore, acute thrombophlebitis – inflammation of a vein with clot formation – is strictly contraindicated․ MLD could potentially dislodge the clot, leading to a pulmonary embolism, a life-threatening complication․ Careful patient screening is essential; individuals with a history of heart failure or angina require medical clearance before undergoing MLD to ensure their safety and prevent exacerbation of their condition․
Severe Cardiac Insufficiency
Severe cardiac insufficiency is a definitive contraindication for Manual Lymphatic Drainage (MLD)․ This condition signifies the heart’s inability to pump sufficient blood to meet the body’s needs, creating a delicate physiological balance․ MLD’s fluid mobilization, even with gentle techniques, can overwhelm a failing heart․
The increased circulatory demand triggered by lymphatic drainage may exacerbate symptoms like shortness of breath and edema․ Introducing additional fluid shifts places an unsustainable burden on the compromised cardiac function․ Prioritizing cardiac stability is paramount; MLD should only be considered after thorough medical evaluation and clearance from a cardiologist, ensuring the patient’s cardiovascular system can tolerate the treatment․
Unstable Angina
Unstable angina represents a critical contraindication to Manual Lymphatic Drainage (MLD)․ This condition signifies unpredictable chest pain due to reduced blood flow to the heart, often a precursor to a heart attack․ MLD, even when gentle, stimulates circulation and increases cardiac workload․
This increased demand can precipitate or worsen angina symptoms, potentially leading to serious cardiovascular events․ The body’s physiological response to MLD – including subtle changes in blood pressure and heart rate – could destabilize the delicate balance in someone with unstable angina․ Absolute avoidance of MLD is essential until the condition is stabilized through appropriate medical intervention and a cardiologist provides explicit clearance․
Acute Thrombophlebitis
Acute thrombophlebitis, characterized by inflammation and clot formation in a vein, is a firm contraindication for Manual Lymphatic Drainage (MLD)․ Applying MLD techniques to an affected area risks dislodging the clot, initiating a potentially life-threatening pulmonary embolism;
The manipulation inherent in MLD could exacerbate inflammation and further compromise venous circulation․ Even indirect pressure near the thrombotic site is inadvisable․ Prioritization of medical management – including anticoagulation therapy – is paramount․ MLD should only be considered after complete resolution of the thrombophlebitis, confirmed by a physician, and with careful consideration of the individual’s overall health status․
C․ Acute Inflammatory Conditions
Acute inflammatory conditions represent significant contraindications for Manual Lymphatic Drainage (MLD)․ This encompasses conditions like acute arthritis and acute gout, where the body is actively fighting inflammation․ Applying MLD could intensify the inflammatory response, worsening pain and potentially spreading the inflammation to unaffected areas․
MLD’s stimulation of circulation might exacerbate the existing inflammatory cascade․ It’s crucial to allow the acute phase to subside before considering any lymphatic work․ Medical management focusing on reducing inflammation – through medication or other interventions – takes precedence․ MLD should only be contemplated once the acute inflammation has resolved, and with physician approval․
Acute Arthritis
Acute arthritis is a definitive contraindication for Manual Lymphatic Drainage (MLD)․ During an acute flare-up, joints are intensely inflamed, swollen, and painful․ Applying MLD to these areas could significantly worsen symptoms and potentially cause further damage․
The gentle, rhythmic movements of MLD, while generally beneficial, can stimulate circulation and potentially increase inflammatory mediators within the affected joint․ This heightened activity could amplify pain and swelling․ It’s vital to prioritize reducing the acute inflammation through medical intervention before considering MLD․ Treatment should focus on pain management and allowing the joint to rest and recover before any manual therapy is applied․
Acute Gout
Acute gout represents a significant contraindication to Manual Lymphatic Drainage (MLD)․ This condition involves sudden, severe attacks of pain, redness, and tenderness in joints, often the big toe, caused by uric acid crystal deposits․
Applying MLD during an acute gout flare-up could exacerbate the inflammation and intensify the excruciating pain․ The manipulation, even gentle, might disturb the crystal deposits and trigger a more intense inflammatory response․ Prioritizing medical management to reduce uric acid levels and control the acute attack is paramount․ MLD should only be considered once the acute phase has subsided and the joint has stabilized, under the guidance of a healthcare professional․
II․ Relative Contraindications
Relative contraindications for Manual Lymphatic Drainage (MLD) require careful consideration and individualized assessment․ These conditions don’t automatically exclude MLD, but necessitate caution and potential modification of the technique or deferral until stability is achieved․
Cancer patients with active malignant tumors or undergoing treatment, particularly post-carcinoma edema, require specialized protocols and physician approval․ Untreated metastasis is a strong relative contraindication․ Systemic diseases like hepatic cirrhosis with ascites and renal failure demand cautious approach due to fluid balance concerns․ Similarly, thyroid dysfunction needs evaluation․ Inflammatory and autoimmune disorders, like chronic inflammation, rheumatoid arthritis flare-ups, and SLE, also warrant careful assessment before proceeding with MLD․
A․ Cancer & Oncology Patients
Manual Lymphatic Drainage (MLD) in cancer and oncology patients requires extreme caution․ Active malignant tumors represent a relative contraindication, as MLD could theoretically promote metastasis, though evidence is limited․ Edema following carcinoma treatment, such as post-surgical swelling or radiation-induced lymphedema, necessitates a specialized approach, often requiring a trained lymphedema therapist․
Untreated metastasis is a significant contraindication, as MLD could potentially spread cancerous cells․ Always obtain physician clearance before treating oncology patients․ Modifications to technique, such as proximal focus and gentle pressure, are often necessary․ Careful monitoring for any adverse reactions is paramount throughout the treatment process․
Active Malignant Tumors
Active malignant tumors pose a relative contraindication to Manual Lymphatic Drainage (MLD)․ The primary concern revolves around the potential, albeit debated, risk of promoting cancer cell dissemination through lymphatic pathways․ While definitive evidence remains limited, caution dictates avoiding direct treatment over or near known tumor sites․
MLD’s effect on metastasis is not fully understood; therefore, physician clearance is absolutely essential․ If treatment is considered, it should only be performed by a highly skilled therapist with oncology experience․ Gentle, proximal techniques are favored, avoiding deep pressure․ Thorough documentation and vigilant monitoring for any adverse effects are crucial throughout the treatment process․
Edema Following Carcinoma Treatment
Edema frequently develops post-carcinoma treatment, often due to surgical lymph node removal or radiation therapy․ While Manual Lymphatic Drainage (MLD) can be beneficial for managing this edema, it requires careful consideration․ Direct treatment should be avoided in areas immediately post-surgery until adequate healing occurs, typically around six weeks, as per medical advice․
Post-mastectomy patients with lymph node removal necessitate a specialized approach, demanding a therapist experienced in lymphedema management․ MLD can help redirect fluid flow, but aggressive techniques are contraindicated․ Physician approval is paramount, and treatment should be integrated with compression therapy and exercise for optimal results, always prioritizing patient safety․
Untreated Metastasis
Untreated metastasis represents a significant contraindication for Manual Lymphatic Drainage (MLD)․ Manipulating the lymphatic system in the presence of active, undiagnosed, or untreated metastatic cancer carries substantial risk․ MLD could potentially stimulate lymphatic spread of cancerous cells, accelerating disease progression․
Prior to initiating MLD, thorough medical evaluation is essential to rule out metastasis․ If cancer is present, treatment should be coordinated with an oncologist․ MLD may be considered after active treatment (surgery, chemotherapy, radiation) and with explicit medical clearance, focusing on symptom management, not curative intent․ Caution and careful assessment are vital to avoid unintended consequences․
B․ Systemic Diseases
Systemic diseases pose notable contraindications to Manual Lymphatic Drainage (MLD)․ Conditions like hepatic cirrhosis with ascites significantly impair the body’s fluid regulation, making MLD potentially harmful by overloading an already compromised system․ Similarly, renal failure hinders fluid excretion, increasing the risk of edema exacerbation․
Thyroid dysfunction, particularly hyperthyroidism, can alter metabolic rate and fluid balance, necessitating caution․ MLD should be avoided or modified in these cases․ Careful consideration and medical clearance are paramount, as MLD could worsen existing imbalances or interfere with medical management of these complex conditions․

Hepatic Cirrhosis with Ascites
Hepatic cirrhosis with ascites represents a significant contraindication for Manual Lymphatic Drainage (MLD)․ This condition involves severe liver damage and fluid accumulation in the abdominal cavity (ascites), disrupting normal fluid balance․ Applying MLD could overwhelm the compromised liver’s ability to process fluids, potentially worsening ascites and leading to complications․
The altered portal hypertension and impaired protein synthesis associated with cirrhosis create a fragile physiological state․ MLD’s stimulation of lymphatic flow might exacerbate fluid shifts and increase the risk of complications like spontaneous bacterial peritonitis․ Therefore, MLD is generally avoided in patients with this condition, prioritizing medical management focused on liver function and fluid control․
Renal Failure
Renal failure constitutes a relative contraindication for Manual Lymphatic Drainage (MLD) due to the kidneys’ crucial role in fluid and electrolyte balance․ Impaired kidney function diminishes the body’s capacity to effectively manage fluid shifts induced by lymphatic drainage․ Applying MLD could overload the system, potentially leading to edema, electrolyte imbalances, and increased strain on the already compromised kidneys․
Patients with renal failure often experience fluid retention and may be on fluid restrictions․ MLD’s stimulation of lymphatic flow could disrupt this delicate balance․ Careful consideration and medical clearance are essential before considering MLD, focusing on the severity of renal impairment and overall patient stability․
Thyroid Dysfunction
Thyroid dysfunction, encompassing both hypothyroidism and hyperthyroidism, presents a relative contraindication for Manual Lymphatic Drainage (MLD)․ Thyroid hormones significantly regulate metabolic rate and fluid balance within the body․ Imbalances can affect lymphatic function and overall physiological responses to MLD․
In hypothyroidism, slowed metabolism may impair the body’s ability to process mobilized fluids effectively․ Conversely, hyperthyroidism can lead to increased metabolic activity and potential overstimulation․ MLD could exacerbate these existing imbalances․ A thorough medical evaluation, including thyroid hormone levels, is vital before initiating MLD, ensuring patient safety and avoiding adverse effects․
C․ Inflammatory & Autoimmune Disorders
Inflammatory & autoimmune disorders necessitate caution with Manual Lymphatic Drainage (MLD)․ Chronic inflammation, regardless of origin, can compromise lymphatic vessel integrity and function, potentially worsening symptoms with stimulation․ Rheumatoid Arthritis (RA), during active flare-ups, presents a relative contraindication due to heightened inflammation and joint sensitivity; MLD could exacerbate pain and swelling․
Similarly, Systemic Lupus Erythematosus (SLE), an autoimmune disease affecting multiple organ systems, requires careful consideration․ MLD’s impact on immune responses is unpredictable in SLE patients․ A physician’s clearance and a gentle, modified approach, avoiding areas of active inflammation, are crucial for minimizing risks․
Chronic Inflammation
Chronic inflammation represents a significant relative contraindication for Manual Lymphatic Drainage (MLD)․ Prolonged inflammatory states, stemming from various underlying conditions, can compromise the lymphatic system’s ability to effectively drain fluids․ MLD, while intended to aid drainage, could potentially exacerbate inflammation by mobilizing inflammatory mediators within the tissues․
The increased circulation stimulated by MLD might worsen symptoms in individuals with pre-existing chronic inflammatory conditions․ Careful assessment of the inflammatory process, its location, and severity is paramount․ A modified approach, focusing on areas without active inflammation, or deferral of treatment until the inflammatory response is better controlled, may be necessary․

Rheumatoid Arthritis (Active Flare-Ups)
Rheumatoid Arthritis (RA), particularly during active flare-ups, poses a relative contraindication to Manual Lymphatic Drainage (MLD)․ The heightened inflammation and joint sensitivity characteristic of RA flares render the tissues extremely vulnerable․ Applying MLD during these periods could intensify pain, increase inflammation locally, and potentially exacerbate joint damage․
While MLD can be beneficial for managing edema associated with RA in stable phases, it’s crucial to avoid treatment when the disease is actively flaring․ A thorough assessment of the patient’s current RA status, including disease activity scores and symptom severity, is essential․ Treatment should be postponed until the flare subsides and inflammation is better managed with conventional medical therapies․
Systemic Lupus Erythematosus (SLE)
Systemic Lupus Erythematosus (SLE) represents a significant relative contraindication for Manual Lymphatic Drainage (MLD)․ This chronic autoimmune disease causes widespread inflammation affecting various organ systems․ MLD, while generally gentle, could potentially trigger or worsen systemic inflammatory responses in individuals with active SLE․
The unpredictable nature of SLE flares necessitates caution․ Applying MLD during a flare-up might exacerbate symptoms, including fatigue, joint pain, and skin rashes․ Careful consideration of disease activity, organ involvement, and current medication regimen is paramount․ Consultation with the patient’s rheumatologist is crucial before considering MLD, ensuring it won’t interfere with their treatment plan or compromise their health․
III․ Specific Considerations & Precautions
Specific considerations are vital when assessing Manual Lymphatic Drainage (MLD) candidacy․ Patients with Congestive Heart Failure require careful evaluation, as MLD could potentially overload the circulatory system․ A history of Deep Vein Thrombosis (DVT) necessitates caution, as MLD might dislodge clots, though this risk is debated․
Skin conditions like open wounds or ulcers and active dermatitis are contraindications due to infection risk and potential irritation․ Post-surgical patients, especially within six weeks, need clearance, as MLD could disrupt healing․ Post-mastectomy with lymph node removal demands a specialized, gentle approach, often requiring a trained lymphedema therapist․
A․ Lymphatic System Compromise
Lymphatic system compromise presents significant cautions for Manual Lymphatic Drainage (MLD)․ Congestive Heart Failure patients require meticulous assessment; MLD’s fluid mobilization could exacerbate cardiac strain․ A prior diagnosis of Deep Vein Thrombosis (DVT) warrants careful consideration, as manipulation might theoretically dislodge a clot, though evidence is debated․
Individuals with impaired lymphatic function, even without a DVT history, may experience adverse reactions․ Pre-existing lymphatic fragility demands a gentle, modified technique․ Always prioritize patient safety and thoroughly evaluate cardiovascular health before initiating MLD, especially in cases of compromised lymphatic pathways․
Congestive Heart Failure
Congestive Heart Failure (CHF) represents a notable contraindication, or requires extreme caution, for Manual Lymphatic Drainage (MLD)․ MLD’s mobilization of fluids can significantly increase circulatory volume, potentially overloading an already stressed cardiovascular system․ This increased fluid load can exacerbate edema and worsen heart failure symptoms․
While some practitioners believe gentle MLD can assist fluid balance in CHF, it necessitates a physician’s clearance and a highly skilled therapist․ Careful monitoring during treatment is essential, watching for signs of distress․ Generally, MLD is avoided in acute CHF or unstable cardiac conditions, prioritizing cardiac stability above lymphatic drainage․
History of Deep Vein Thrombosis (DVT)

A history of Deep Vein Thrombosis (DVT) warrants significant caution when considering Manual Lymphatic Drainage (MLD)․ While MLD isn’t directly contraindicated, the risk of dislodging a residual clot, even a previously treated one, exists․ Mobilizing fluids could potentially carry a small clot to the lungs, causing a pulmonary embolism – a life-threatening complication․

Therefore, a thorough medical evaluation is paramount․ MLD should only be performed with explicit physician approval and a detailed understanding of the DVT’s history, location, and treatment․ Proximal DVT (closer to the torso) presents a higher risk․ Gentle, distal MLD (further from the torso) might be considered, but constant monitoring for any signs of discomfort or changes in circulation is crucial․
B․ Skin Conditions

Manual Lymphatic Drainage (MLD) is generally not recommended in the presence of certain skin conditions․ Open wounds or ulcers represent a clear contraindication, as MLD could exacerbate inflammation and impede the healing process, potentially introducing infection․ Similarly, active dermatitis – characterized by inflamed, itchy skin – is a concern․
MLD could spread the inflammation or compromise the skin barrier, worsening the condition․ Compromised skin integrity increases susceptibility to infection․ Even seemingly minor skin irritations should be carefully assessed․ A physician’s clearance is essential before proceeding with MLD on areas affected by skin conditions, ensuring the treatment won’t negatively impact skin health or recovery․
Open Wounds or Ulcers
Manual Lymphatic Drainage (MLD) is strictly contraindicated when open wounds or ulcers are present․ These breaches in the skin’s protective barrier significantly elevate the risk of introducing bacteria and causing infection․ The gentle, rhythmic movements of MLD can inadvertently spread pathogens directly into the wound site, hindering the natural healing process․
Furthermore, MLD’s effect on fluid dynamics could disrupt the delicate balance required for proper wound closure․ Increased local circulation, while generally beneficial, might exacerbate inflammation around the ulcer․ Thorough assessment and complete wound healing are prerequisites before considering MLD in the affected area․ Prioritizing wound care and infection prevention is paramount․
Active Dermatitis
Manual Lymphatic Drainage (MLD) should be avoided in areas exhibiting active dermatitis․ This inflammatory skin condition, characterized by redness, itching, and potential blistering, represents a compromised skin barrier․ Applying MLD techniques could further irritate the inflamed tissue, intensifying discomfort and potentially spreading the dermatitis to unaffected areas․
The manipulation involved in MLD might disrupt the skin’s natural protective function, increasing susceptibility to secondary infections․ It’s crucial to allow the dermatitis to subside and the skin to heal before initiating any lymphatic drainage treatment․ Addressing the underlying cause of the dermatitis and implementing appropriate skincare are essential prior to considering MLD․
C․ Post-Surgical Considerations
Post-surgical patients require careful evaluation before Manual Lymphatic Drainage (MLD) is considered․ Generally, waiting at least six weeks post-surgery is recommended to allow initial healing and minimize risks․ Recent surgical sites are vulnerable to infection and fluid imbalances, which MLD could exacerbate․
Post-mastectomy cases, particularly those involving lymph node removal, necessitate a specialized approach․ Disrupted lymphatic pathways require a tailored MLD protocol administered by a trained therapist experienced in post-cancer care․ Premature or improper MLD can impede healing, increase lymphedema risk, and compromise surgical outcomes․ Thorough communication with the surgical team is paramount․
Recent Surgery (within 6 weeks)
Manual Lymphatic Drainage (MLD) is generally contraindicated within six weeks of any surgical procedure․ This period is critical for tissue repair and wound stabilization; MLD could disrupt these processes․ Surgical trauma inherently impacts the lymphatic system, creating inflammation and potential fluid accumulation․
Applying MLD too soon can overwhelm the healing tissues, increasing the risk of infection, hematoma formation, and delayed wound closure․ The body needs time to establish new lymphatic pathways and regain homeostasis․ Exceptions are rare and require direct physician approval, considering the specific surgery and individual patient factors․ Prioritizing proper healing is essential before initiating lymphatic work․
Post-Mastectomy with Lymph Node Removal (requires specialized approach)
Post-mastectomy patients, particularly those undergoing axillary lymph node dissection, require a highly specialized approach to Manual Lymphatic Drainage (MLD)․ Routine MLD is often contraindicated immediately post-surgery due to increased risk of lymphedema․ The removal of lymph nodes compromises lymphatic drainage in the affected arm․
However, carefully applied, gentle techniques by a certified lymphedema therapist can be beneficial after adequate healing and with physician clearance․ This specialized MLD focuses on redirecting lymphatic flow and promoting the growth of collateral pathways․ Self-care education is vital․ Untrained application can exacerbate lymphedema risk; therefore, expert guidance is paramount for safe and effective management․